Where the path of innovation leads
Professor Frank Gannon
Research should have consequences, and a link with business to obtain investment for rigorous clinical trials sparks great Australian innovation

Nobel prizes for medical research usually go to researchers who have defined a new cellular process or structure. Increasingly, Nobel Prizes announcements stress the potential benefits to society, and the step from innovative research to innovative products. Likewise, most funding agencies and governments expect a return on investment, something I am acutely aware of as the director of a medical research institute. The task with which we are charged does not end when we publish a paper: it has to be carried through to the clinic or to society.
When we start on a path of innovation, we may have no idea where it will lead or what benefits it will bring. Of the many examples from my time at QIMR Berghofer Medical Research Institute, none better illustrates this than revolutionary new immunotherapies developed in the laboratory of Rajiv Khanna and his colleague Corey Smith. The end point has been exciting new treatments for cancers and auto-immune diseases. But we should start at the beginning, more than 25 years ago, when Rajiv, then a young researcher joined the laboratory of Denis Moss. Building on Denis’ pioneering work understanding how the immune system controlled Epstein-Barr Virus (EBV), Rajiv deciphered how EBV interacted with the immune system. Rajiv reckoned that this knowledge could be exploited to stimulate the immune system in the absence of the active virus itself. Today this is what is happening in our laboratories. Basic research has been translated to new therapies.
The successful development of immunotherapies relies on a deep understanding of how the immune system responds to external challenges. A type of immune cell known as a T cell can be stimulated to respond, for example, to a pathogen.
To illustrate the process, let’s consider the focus of their recent work. EBV commonly causes glandular fever – sometimes known as the ‘kissing disease’ – in Western populations, but for reasons related to genetics, food and the environment, EBV can cause a type of head and neck cancer, nasopharyngeal carcinoma, in people in South-East Asia.
In a world-first clinical trial, Rajiv’s lab, working in conjunction with The Queen Mary Hospital and the University of Hong Kong, brought blood samples from patients in Hong Kong to QIMR Berghofer in Brisbane, where the white blood cells were ‘trained’ to attack specific proteins from EBV present in cancer cells, before being sent back to Hong Kong for treatment of the patients.
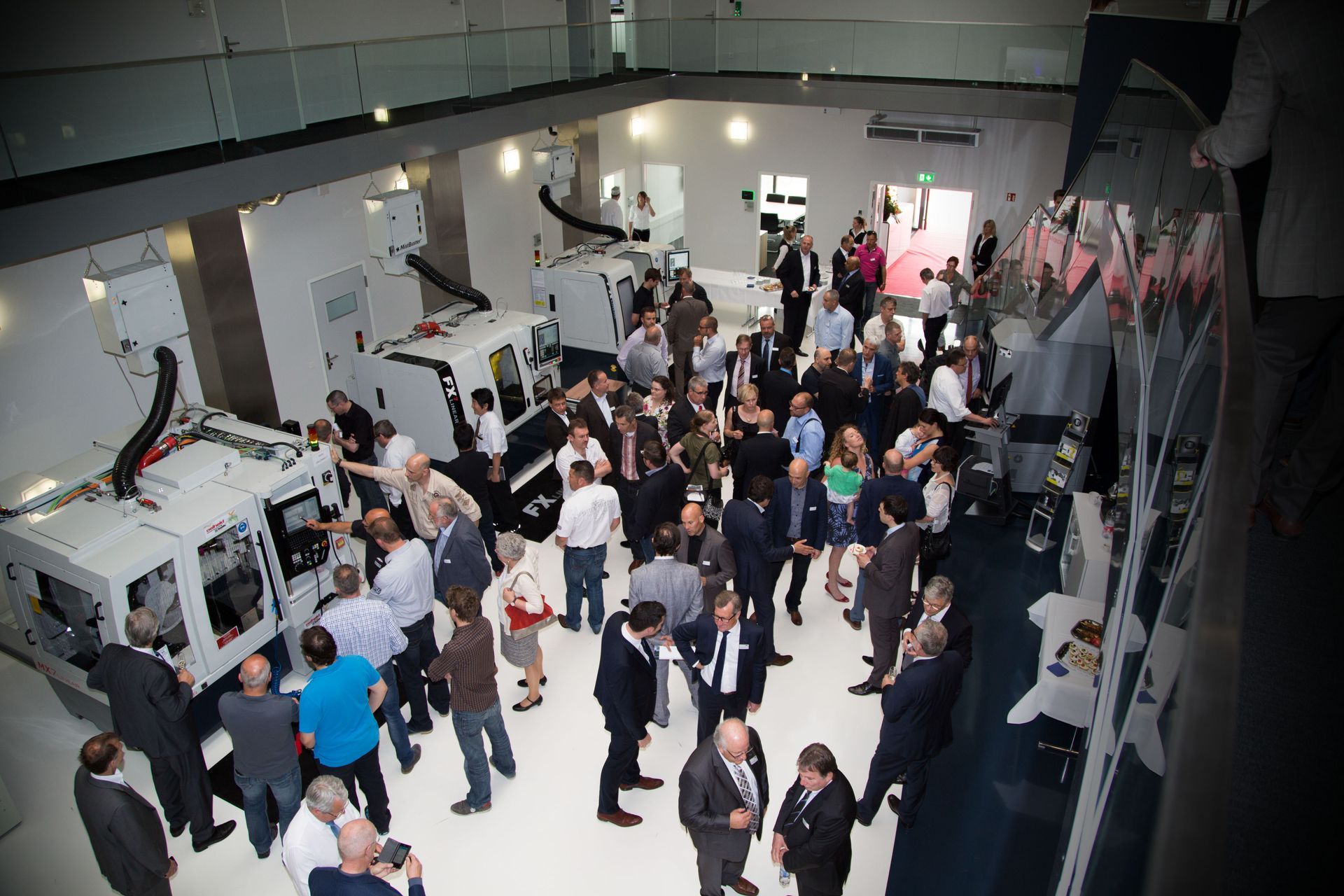
While this sounds straight forward, the immunotherapy had to be produced under clinical-grade conditions, transported internationally and maintained in a pristine state with stringent temperature control and monitoring. For this to happen, QIMR Berghofer had to develop the technology, skill base and infrastructure – a suite of clean rooms built to exacting GMP standards. This cell therapy manufacturing facility, known as Q-Gen, is available to internal and external researchers. Importantly, it addresses a major gap in the global cell therapy manufacturing capacity as the number of cell immunotherapy clinical trials grows annually (more than 250 in 2018).
This initial clinical trial has been expanded to people from South-East Asia now residing in Australia, and has stimulated interest in an unrelated area. A clinician at the Royal Brisbane and Women’s Hospital, Professor Michael Pender, proposed that EBV-infected cells played a role in multiple sclerosis (MS). Using QIMR Berghofer’s capability, Rajiv Khanna undertook an initial pilot study for patients with MS. The data were very promising and, together with the oncology trial results, attracted international interest. US-based cell therapy company Atara Biotherapeutics has now licensed the EBV technology for use in MS patients, with Q-Gen manufacturing the products for the Phase 1 trial. Australia can build on these advanced manufacturing capabilities, given the high skill base and infrastructure now available in Queensland, the strong regulatory framework under which we work and the novelty of the products which we have developed.
These immunotherapy studies using blood products derived from the patient are just a start. QIMR Berghofer is now working with T cells that come from healthy volunteers, allowing the development of off-the-shelf products that can be available on demand. Furthermore, QIMR Berghofer scientists have expanded the range of products to include other viruses, such as cytomegalovirus (CMV), a common virus that can kill immune-suppressed people. Transplant surgery usually requires suppression of the patient’s immune system to stop it attacking the transplanted material. This very suppression may allow viruses such as CMV to run rampant. In one case, a child who had received a transplant developed a severe infection that threatened his sight, and could have taken his life. Immunotherapy targeting CMV was used to successfully treat this child. A clinical trial has recently been successfully completed to treat adult organ transplant patients who had CMV complications, and a new study is being initiated to address CMV and other post-operative viral infections in children receiving transplant. Immunotherapy targeting CMV has also been expanded to treat the deadly brain cancer, glioblastoma. CMV might not cause glioblastoma, but it is a frequent bystander and therefore a potential target for effective treatment.
The road from the initial work on these viruses has been decades long. It required persistent research to refine the initial discoveries. It was underpinned by a very significant understanding of the immune system. Links with clinicians were essential to bring the early stage research through to the clinic. Significant investment was required to ensure that the products could be manufactured at QIMR Berghofer. The attraction of international investment adds to Australia’s economic strength and there is great potential for more. Each step has been driven by an environment and individuals committed to innovation.
We at QIMR Berghofer believe research should have consequences. We believe in linking with business to obtain the required investment, particularly for clinical trials. And we believe the rigor of these trials makes them great Australian innovations. A Nobel Prize was awarded in 2008 for the discovery that a virus caused cancers. The Nobel Prize in 2018 related to the role of T cells as an immunotherapy. The translation of such fundamental discoveries is at the heart of continued innovation. We at QIMR Berghofer are pleased to be part of that continuum.

In 2016 I published a blog article titled Moonshots for Australia: 7 For Now. It’s one of many I have posted on business and innovation in Australia. In that book, I highlighted a number of Industries of the Future among a number of proposed Moonshots. I self-published a book, Innovation in Australia – Creating prosperity for future generations, in 2019, with a follow-up COVID edition in 2020. There is no doubt COVID is causing massive disruption. Prior to COVID, there was little conversation about National Sovereignty or supply chains. Even now, these topics are fading, and we remain preoccupied with productivity and jobs! My motivation for this writing has been the absence of a coherent narrative for Australia’s business future. Over the past six years, little has changed. The Australian ‘psyche’ regarding our political and business systems is programmed to avoid taking a long-term perspective. The short-term nature of Government (3 to 4-year terms), the short-term horizon of the business system (driven by shareholder value), the media culture (infotainment and ‘gotcha’ games), the general Australian population’s cynical perspective and a preoccupation with a lifestyle all create a malaise of strategic thinking and conversation. Ultimately, it leads to a leadership vacuum at all levels. In recent years we have seen the leadership of some of our significant institutions failing to live up to the most basic standards, with Royal Commissions, Inquiries and investigations consuming excessive time and resources. · Catholic Church and other religious bodies · Trade Unions · Banks (and businesses generally, take casinos, for example) · the Australian Defence Force · the Australian cricket teams · our elected representatives and the staff of Parliament House As they say, “A fish rots from the head!” At best, the leadership behaviour in those institutions could be described as unethical and, at worst….just bankrupt! In the last decade, politicians have led us through a game of “leadership by musical chairs” – although, for now, it has stabilised. However, there is still an absence of a coherent narrative about business and wealth creation. It is a challenge. One attempt to provide such a narrative has been the Intergenerational Reports produced by our federal Government every few years since 2002. The shortcomings of the latest Intergenerational Report Each Intergenerational Report examines the long-term sustainability of current government policies and how demographic, technological, and other structural trends may affect the economy and the budget over the next 40 years. The fifth and most recent Intergenerational Report released in 2021 (preceded by Reports in 2002, 2007, 2010 and 2015) provides a narrative about Australia’s future – in essence, it is an extension of the status quo. The Report also highlights three key insights: 1. First, our population is growing slower and ageing faster than expected. 2. The Australian economy will continue to grow, but slower than previously thought. 3. While Australia’s debt is sustainable and low by international standards, the ageing of our population will pressure revenue and expenditure. However, its release came and went with a whimper. The recent Summit on (what was it, Jobs and Skills and productivity?) also seems to have made the difference of a ‘snowflake’ in hell in terms of identifying our long-term challenges and growth industries. Let’s look back to see how we got here and what we can learn. Australia over the last 40 years During Australia’s last period of significant economic reform (the late 1980s and early 1990s), there was a positive attempt at building an inclusive national narrative between Government and business. Multiple documents were published, including: · Australia Reconstructed (1987) – ACTU · Enterprise Bargaining a Better Way of Working (1989) – Business Council of Australia · Innovation in Australia (1991) – Boston Consulting Group · Australia 2010: Creating the Future Australia (1993) – Business Council of Australia · and others. There were workshops, consultations with industry leaders, and conferences across industries to pursue a national microeconomic reform agenda. Remember these concepts? · global competitiveness · benchmarking · best practice · award restructuring and enterprising bargaining · training, management education and multiskilling. This agenda was at the heart of the business conversation. During that time, the Government encouraged high levels of engagement with stakeholders. As a result, I worked with a small group of training professionals to contribute to the debate. Our contribution included events and publications over several years, including What Dawkins, Kelty and Howard All Agree On – Human Resources Strategies for Our Nation (published by the Australian Institute of Training and Development). Unfortunately, these long-term strategic discussions are nowhere near as prevalent among Government and industry today. The 1980s and 1990s were a time of radical change in Australia. It included: · floating the $A · deregulation · award restructuring · lowering/abolishing tariffs · Corporatisation and Commercialisation Ross Garnaut posits that the reforms enabled Australia to lead the developed world in productivity growth – given that it had spent most of the 20th century at the bottom of the developed country league table. However, in his work, The Great Reset, Garnaut says that over the next 20 years, our growth was attributable to the China mining boom, and from there, we settled into “The DOG days” – Australia moved to the back of a slow-moving pack! One unintended consequence of opening our economy to the world is the emasculation of the Australian manufacturing base. The manic pursuit of increased efficiency, lower costs, and shareholder value meant much of the labour-intensive work was outsourced. Manufacturing is now less than 6% of our GDP , less than half of what it was 30 years ago!