ResMed’s quest for improved sleep health
ResMed founder and chairman Peter Farrell depicts the 40-year evolution of sleep apnea treatment, what’s next, and how well Australians sleep compared to the rest of the world

Like paying taxes and death, sleep is something that affects all of us. But how would you rate the overall awareness and appreciation Australians have of sleep as, along with a good diet and physical exercise, one of the three key pillars for public health? Causal factors and solutions for improvement?
PF: Compared to the rest of the world, I think Australians probably have a higher-than-average awareness of sleep and obstructive sleep apnea (OSA) thanks to the far-reaching research that’s been conducted and promoted nationwide, celebration of Colin Sullivan, University of Sydney professor, who invented the nasal continuous positive airway pressure (PAP) machine in the early 1980s, and high visibility of ResMed, world leader in connected solutions for treating sleep apnea and an ASX15 company.
However, in terms of where awareness should be, it’s still too low for Australians as it is everywhere else. According to Lancet Respiratory Medicine, over 936 million people worldwide have sleep apnea – including over 2.9 million Australians. Over 80 per cent are undiagnosed.
We know that leaving sleep apnea untreated – the nightly toll these cyclical suffocations have on our body that should be resting – puts us at 2 to 3 times higher risk for heart attacks or strokes, impacts our daily energy, mood, safety while driving or at work, long-term mental health, and so on. Our sleep health is very much tied to every facet of our overall health and wellbeing.
What is the relationship between sleep and the other two other pillars of public health? Has this been studied and reported on?
PF: The links between sleep and the other two pillars – nutrition and physical exercise – are very strong. Simply put: You can’t optimize your healthy eating or your exercise goals without a good night’s sleep.
If you don’t get enough sleep each night – common recommendations are 7 to 9 hours nightly for adults – you may lack the energy required to exercise as much as you’d like to the next day, as well as focus on work and other important tasks.
Lack of sleep also affects how we eat. First off, if you are sleep deprived and lack energy, your body will likely seek more foods high in carbohydrates and/or fat than you may intend to eat because your body is seeking sources of energy to make up for the energy it didn’t wake up with. What’s worse is sleep deprivation could lead to overeating. A 2013 study published in Psychoneuroendocrinology found sleep-deprived people wake up with higher feelings of hunger and plasma ghrelin levels, which are linked to overeating.
So not only does good sleep restore our bodily functions and refill our energy tanks for the day ahead, it also enables us to best tend to the other important pillars that help sustain our overall health.
Why is sleep so important to Australia’s national interests and its “socio-economic scorecard”? How much do sleeping disorders hurt the national economy and society more broadly? (productivity, domestic violence, road toll, poverty, mental health, etc.)?
PF: A nation’s collective sleep hygiene is key to this scorecard. Sleep deprivation is tied to work absenteeism, presenteeism – which just means you’re at work but not working to your full potential – workplace, and roadway accidents and deaths.
Sleep is also key to our mental health: Sleep deprivation can negatively impact our moods, which can in turn affect the relationships we have with everyone around us. And there’s long-term implications for mental health, too. A 2008 Sleep Medicine Reviews study found sleep disruptions can increase your risk of developing depression. There’s a specific link between depression and obstructive sleep apnea: 1 in 5 people with depression are believed to have OSA, according to the U.S. National Sleep Foundation.
There are profound benefits for individuals and whole societies in improving our sleep and collectively prioritizing good sleep – and huge risks not only to being sleep deprived but also not understanding the effects of that.
Are Australians overall good sleepers? Are there reliable, current, statistics available on sleeping disorder prevalence? Is there a sleeping disorder epidemic in Australia or a risk of one in the coming decade with an ageing population? What is the current trend / dynamic?
PF: Australians get an average 6.8 hours per night, according to ResMed’s own Global Sleep Surveys taken in March 2022. Marginally below 7 to 9 hours per night, not all that bad. But there are two big caveats. One, “average” implies half of Australians are getting less or even far less than that amount, and I urge any of those folks to prioritise sleep and make time for it that can pay dividends in the short and long term for their health and quality of life.
And two, it is estimated that at least 3 million Australians have sleep apnea, many of them undiagnosed and untreated. Those millions of people may think they’re getting 7 to 9 hours, when in fact their bodies could be waking dozens or hundreds of times a night to prevent mini sleep suffocations caused by their apneas. For these folks, the key to restoring and optimizing their sleep begins with diagnosing their condition and treating it at home.
Does Australia as a whole invest much / enough into sleeping disorders relative to its prevalence and severity? How does this compare with other rich western economies?
PF: The western world is ahead of the rest of the world and focusing on the importance of getting a good night’s sleep. However, there is still not enough focus on sleep in general. I’m heartened to see concerted efforts by ResMed and independent universities and researchers to boost general sleep awareness across Asia, Latin America, as well as in more established markets.
What are some of the latest notable cutting-edge R&D findings, here and globally, related to sleeping disorders from cause, treatment, and cure perspectives?
PF: Sleep apnea is an important component of chronic disease. If the sleep apnea is left untreated, many damaging conditions may occur such as hypertension, and eventually type 2 diabetes. There are many other connections between untreated OSA and chronic diseases. The bottom line is that OSA needs treatment otherwise one’s health will significantly deteriorate.
How and where has ResMed expanded scientific knowledge of sleeping disorders in the last 1-2 years since your original article on this subject was prepared? What are some surprising or even shocking facts and figures?
PF: We can now say that PAP treatment has helped people live longer. The landmark ALASKA study presented at last year’s European Respiratory Society Congress in France showed people with OSA who stayed on therapy were 39 per cent more likely to survive over a 3-year period than OSA patients who didn’t. There were over 176,000 people in this study – and the results held regardless of age, preexisting conditions, overall health, or cause of death. It goes to show how important diagnosis and treatment of this disease really are.
There’s more coming out of ALASKA and other studies ResMed conducts. We are truly leaders not just in helping the world treat these diseases but in understanding them – how common they are, their effects on other diseases and facets of our health, and what types of digital solutions and other interventions work best in terms of engaging people to start and stay on treatment.
Since last we spoke, Lancet Respiratory Medicine had just published ResMed’s latest global prevalence of sleep apnea – almost a billion people worldwide. This is a staggering number. Some 3 million Australians are believed to have it. Since the study came out, it has become one of the most cited resources of prevalence, and people are becoming more aware of how big an issue this is if left untreated OSA is.
ResMed invests around 7 to 8 per cent of company revenue into R&D to support future growth. What are some notable recent R&D findings? Is there more of a focus on incremental improvements to existing ResMed products or disruptive products? Why should sleeping disorder sufferers be excited about the next 5-10 years of innovation at ResMed?
PF: R&D funds go into improving every aspect of the user’s experience. We continue to push the envelope on digital solutions designed to engage, motivate, and empower users to track and improve their own treatment. This is true across much of healthcare, but ResMed has long been a leader in this space – today there are nearly 18 million connected ResMed devices on bedside tables across 140+ countries. Our latest PAP platform AirSense 11 features new digital solutions, one for helping guide new users onto treatment – in those first few days it’s vital for someone to have confidence in the treatment and embrace it. The other automatically checks in with users at 30, 60, 90 days, and so on to see how they’re doing and suggest advice if needed.
And of course, we’re always striving to make the therapy itself smaller, quieter, more comfortable. PAP treatment just turned 40, and in four short decades we’ve made leaps and bounds – from a 10 kilograms machine the size (and noise) of a pool air filter to the ResMed AirMini, which has waterless humidification, runs off your phone, and itself is about the size of an iPhone – the world’s smallest PAP to date, weighing about 0.07 pounds or 0.032 kilograms. There’s much more to unlock; we’re not done improving on these technologies.
Can ResMed’s historic and anticipated contribution to humanity be quantified/estimated?
PF: First off, the last two years have been dominated by the COVID-19 pandemic and during the past year, global supply chain challenges, and a major competitor recall in our industry. It is undisputed that the need for ventilators at the outset of COVID-19 was massive and critical, and I’m incredibly proud and amazed at ResMed’s – and frankly all leading ventilator makers’ – ability to produce what we did to meet the world’s demand and save countless lives. ResMed itself pivoted its whole business to make ventilators – it’s usually less than 10 per cent of our business – and set a record: hundreds of thousands of these lifesaving devices were produced in 2020 alone.
Today, ResMed is helping fill an historic need for PAP devices in the wake of global supply shortages and a competitor’s recall. We’re talking with suppliers and their suppliers, in the supply chain to get the chips we need so millions of people worldwide can get the nightly sleep they require.

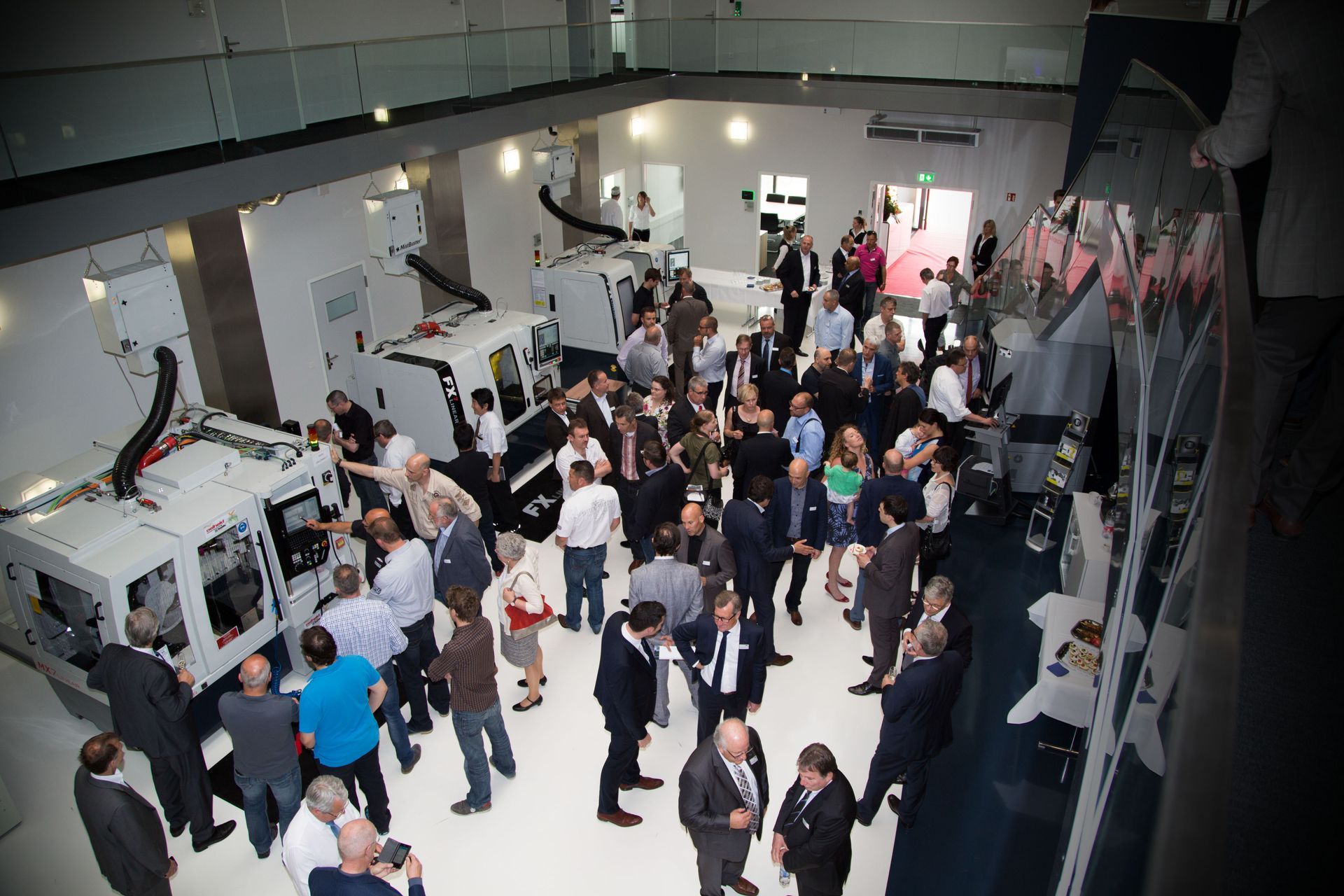
Peter at an event in the early 1990s, when ResMed went by its original name “ResCare.”