Malaria vaccine could offer universal protection
Malaria vaccine trials conducted at James Cook University (JCU) are hoping to prove universally effective against the four types of malaria that infect humans.
If successful, the vaccine has the potential to save hundreds of thousands of lives per year, and prevent millions of susceptible individuals from being infected.
JCU’s Australian Institute for Tropical Health and Medicine (AITHM) has led the efforts to develop a safe, effective and low-cost universal malaria vaccine and has now joined forces with Defence Materials Technology Centre (DMTC) to begin manufacturing and clinical-stage development.
The world’s largest research-based pharmaceutical company Pfizer Hospira and Glycosyn, a global leader in the development and manufacture of active pharmaceutical ingredients have also signed on as partners in the project to assist in both the clinical and manufacturing stages of the project.
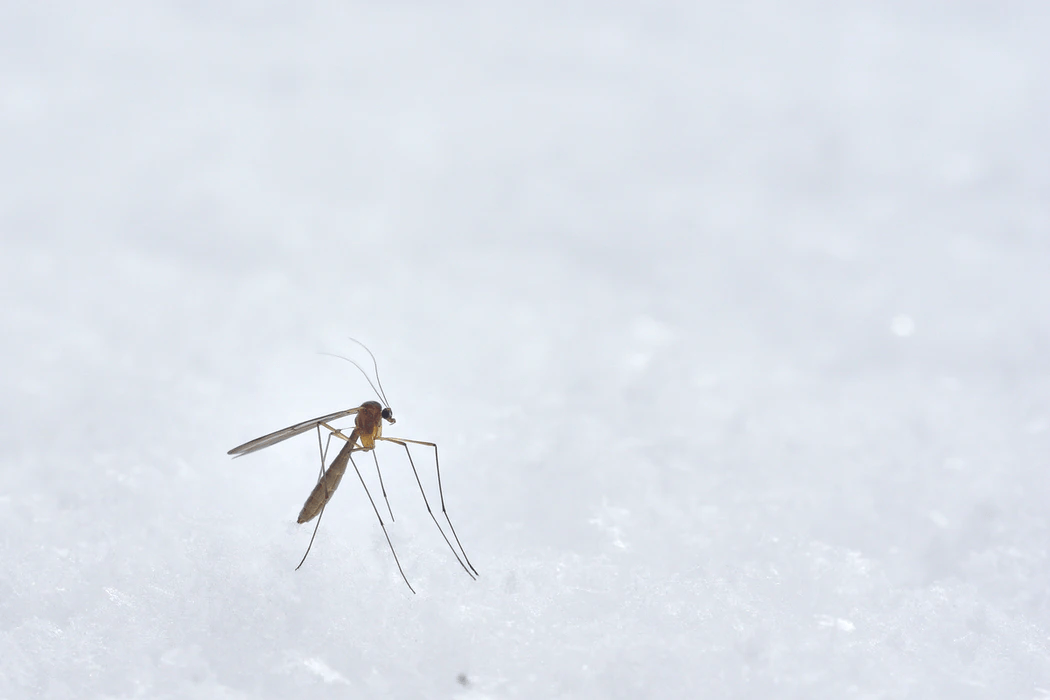
Whilst Australia is relatively malaria-free, an estimated 228 million people were infected with malaria by mosquitoes in 2018 according to the World Health Organisation (WHO).
This figure also includes an estimated 405,000 deaths, 67% of which were children under five years of age, many of whom live in third world countries and tropical regions overseas.
According to Director of the AITHM, Professor Louis Schofield, “there is currently no vaccine that is protective against all strains, species and life cycles of malaria that can prevent both infection and disease transmission”.
However, if the clinical trials bear fruitful results, AITHM’s research efforts may solve this massive global health problem.
The first stage will see JCU complete preclinical toxicology work and the first phase of the clinical stage.
This will include a focus on the development of GPIVax, a carbohydrate-based malaria vaccine candidate that has previously shown strong preclinical effectiveness across all species, strains and life cycle stages of malaria tested to date according to JCU.
“Once the vaccine is proven safe in volunteers, the next stage will be to test its efficacy in preventing malaria,” said Schofield.
This will be achieved through collaboration with neighbouring countries across South East Asia and the South-West Pacific in nations such as the Solomon Islands, Philippines, Thailand and Papua New Guinea.
“We have close ties to scientists and physicians in near neighbouring countries where malaria remains a huge problem and who will collaborate in testing the vaccine in those settings,” said Schofield.
The second stage will see Australia’s limited vaccine development capability improved so high-quality manufacturing capability for biotechnology products is possible and can meet stringent government standards.
According to Schofield, AITHM and JCU are committed to developing and supporting the local Australian biotech manufacturing industry through the manufacturing stage of the vaccine.
Currently, the vaccine is still undergoing regulatory authority compliance measures conducted by the Therapeutic Goods Administration (TGA) but Schofield expects it to be approved for manufacture and clinical purposes mid-2021.
Human trials will begin at Townsville Hospital with volunteers towards the last quarter of 2021 and field trials will begin in affected partner nations early 2022 through the use of both the vaccine and a placebo drug.
“I’ve worked in this field for more than 30 years, I wouldn’t go down this path if I didn’t believe our efforts to produce a safe, effective and universal vaccine for malaria wouldn’t work,” said Schofield.